Fact checked by Wilfred G. Van Gorp, Ph. D., on June 5, 2019 — Written by Shana De Caro & Michael V. Kaplen.
Our goal in creating this guide, is to help you understand epilepsy and seizures, common conditions caused by head and brain injury. This guide is not intended to replace proper medical advice. If you or a loved one think you may have sustained a seizure or suffer from epilepsy, seek the opinion of a medical professional for proper diagnosis.
Seizures aren’t the same for everyone: they are manifested differently for each person. We think of seizures as violent jerking or stiffening of the body with the victims suddenly finding themselves on the ground. Others, however, may experience different physical signs, including visual or hearing disturbances, abnormal electrical sensations or numbness, abruptly waking up, urinary discharge, and even staring blankly into space.
Seizures, no matter their appearances, can cause terrifying experiences and result in physical and psychological consequences for the victim.
The term epilepsy is used to identify individuals who have suffered two or more seizures.1
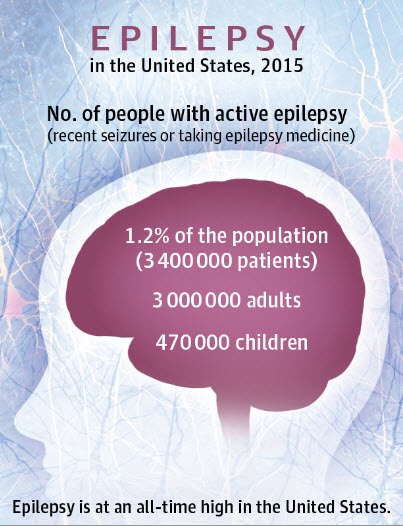
If you or a loved one has been diagnosed with epilepsy, you are not alone. According to the Epilepsy Foundation, approximately 3.4 million Americans suffer from epilepsy.2 This disorder is far more common than most people realize, but it rarely gets the public attention it deserves.
Seizures and resultant epilepsy are often caused by head trauma.3 When seizures are caused by a head or brain injury, it is referred to as post-traumatic epilepsy.4 It is estimated that trauma causes 20% of symptomatic epilepsy.5 Seizures may have other causes, including neurological disorders such as a tumor6 or stroke7. In approximately half of those diagnosed with epilepsy, however, the cause is unknown.8
Epilepsy is generally not diagnosed until one experiences a second seizure, usually within a short time after the first. Given the complex and often mysterious nature of seizures, even the best medical professionals cannot identify epilepsy from just a single occurrence. Seizures can occur within moments, days, weeks, months, or even years following head trauma.9 Seizures occurring shortly after trauma increase the risk for developing further seizures.10
Therefore, when one has a second seizure he or she is faced with a terrifying realization: this may be a permanent part of my life.
Yes, the first time is scary. The second time, however, represents the beginning of a pattern.
For those living with epilepsy, the disorder is not necessarily about the seizures: it is about how the seizures impact daily life. How can I still do well in school? What will happen if a seizure strikes while I am at work? Can I safely live on my own, or do I need a caregiver? Will I be able to drive a car? These are difficult questions people with epilepsy must confront.
You may have many questions about epilepsy. We have assembled this guide to help you find answers to many of the frequent questions about epilepsy, with special consideration of epilepsy caused by a traumatic brain injury. We have also included a list of resources to help guide you through your journey.
If you or a loved one has been diagnosed with epilepsy, you may find it helpful to share this with friends and family, so they may have a better understanding of what epilepsy is, and how it affects your life.
What Is Epilepsy?
Epilepsy is a general term for all seizure disorders.
Epilepsy is not a single seizure. Someone with a single isolated seizure is not epileptic. Epilepsy is generally only diagnosed after someone suffers two seizures within a short time, or experiences multiple seizures without having any before.11
An epileptic seizure is a sudden surge of electrical activity in the brain.12 In epileptic patients, the normal pattern of electrical activity in the brain is disturbed, causing strange sensations, emotions, and behaviors. These electrical impulses in the brain transmit to the muscles, explaining why someone experiencing an epileptic seizure may appear to lose control of his or her body.
There are many forms of seizures, and those undergoing a seizure may display very few visible symptoms. Symptoms of a seizure can range from loss of physical sensation, to whole-body stiffening, to uncontrollable jerking motions. Seizure symptoms can also be pain in the stomach, or extreme mood changes.13
While no cure for epilepsy exists, the condition may be managed through medical, surgical, and other strategies.
Epilepsy in the USA: Facts and Figures

1.2%
of the US population has active epilepsy.
3.47m
adults and children are currently affected.
1 in 26
individuals will develop epilepsy.
Epilepsy is a common disease: it trails only migraine, stroke, and Alzheimer’s as the fourth most common neurologic disease in the country.15 If you combine the number of people with cerebral palsy, muscular dystrophy, multiple sclerosis, and cystic fibrosis, that equals less than half the people diagnosed with epilepsy in the U.S.16
Anyone can develop epilepsy. It can occur in anyone, regardless of age, race, or gender.17
Treatment can be effective, but many cases of epilepsy do not respond positively to treatment. It is estimated that 1 million people in the United States have epilepsy uncontrolled by medication.18
In the most severe cases, people may die from epilepsy. People with epilepsy can die from prolonged seizures (known as status epilepticus) or from Sudden Unexpected Death in Epilepsy (SUDEP). According to the Centers for Disease Control and Prevention (CDC) 1.16 out of every 1,000 epilepsy patients will die from SUDEP each year.19
What Causes Epilepsy and Seizures?
Epilepsy is not contagious.20 This is a common misconception.
Unfortunately, there is much public confusion about this disorder. If you or a loved one has been diagnosed with epilepsy, this can lead to frustration.
What Causes Epilepsy?
Many cases of epilepsy have no clear cause, and those with known causes usually involve an injury to the brain.21
These traceable causes include:
Head Trauma
This could result from a car accident, fall, or other traumatic event, causing brain injury.
Head injuries resulting in skull fractures, and bleeding within the brain (subdural hematoma and intracerebral hematoma) increase the risk of developing a seizure disorder.22
Closed head injuries, where the brain moves within the skull, causing shearing, stretching, and tearing of nerve fibers, can also cause seizures. Studies have found that the risk of epilepsy doubles after a mild head injury, and individuals with a severe head injury are seven times more likely to develop epilepsy.
The risk of developing seizures is elevated for upward of 20 years following a head injury.23
Brain Conditions
This includes brain tumors and strokes (strokes are the leading cause of epilepsy in adults older than 35).24
Infectious Diseases
Such as meningitis, AIDS, and viral encephalitis.25
Prenatal Injury
Babies are sensitive to brain damage that could be caused by an infection in the mother, poor nutrition, or oxygen deficiencies.26
What Triggers An Epileptic Seizure?

Understanding what triggers a seizure is an important part of medical treatment. Through proper medical treatment, seizures may be controlled, but unfortunately, life rarely returns to “normal” for those diagnosed with epilepsy.
For a small portion of those diagnosed with epileptic seizures (roughly 3%) flashing or flickering lights can trigger several types of seizures. This form of epilepsy is photosensitive epilepsy.28 Common triggers, however, are far more ordinary occurrences.
If a loved one has been diagnosed with epilepsy, take time to understand their triggers. Ask if there’s anything you should know when you are with them. Remind them that they are not alone in this journey.
Before the Seizure: Prodromal Symptoms
Hours or even days before a seizure happens, some people with epilepsy may experience “warning signs” known as prodromal symptoms. These symptoms are often described by epilepsy patients as a sensation that something is “off,” such as mood changes.29
The 3 Stages of a Seizure
No matter what the cause or trigger, individuals experiencing a seizure often go through several distinct stages. These stages are named: auras, ictal, and postictal.30
Stage 1: Aural Stage
The aura stage is the beginning of the seizure and often only lasts for seconds or minutes. Not all seizures start with a distinct aura stage, but many do. The symptoms in the aura stage are usually only noticeable by the patient themselves and are not visible to the outside observer.
People experiencing an aura stage often describe abnormal feelings or sensations, such as déjà vu, out-of-body experiences, or “phantom” sounds, tastes, or smells. Aura stages can be accompanied by physical sensations such as dizziness, nausea, headaches, numbness, or lightheadedness. People in the aura stage may experience heightened emotions, such as fear and panic.
Some seizures stop after the aura stage and leave the person aware and able to respond. Other seizures may proceed to other stages.
Stage 2: Ictal Stage
The ictal stage is the seizure itself.
When people think of a seizure, they are typically referring to the ictal stage. If the aura stage is the beginning of the seizure, this is the middle. Intense electrical charges are emitted in the brain. This stage is the actual seizure: the electrical storm is unleashed from your brain throughout your body.
Ictal stage symptoms are not just the tremors or jerking motions that most people associate with someone having a seizure. They can include sensory and cognitive changes similar to the aura stage.
The physical symptoms also vary widely from individual to individual. Some people “blackout,” while others retain consciousness. Even if someone in the ictal stage is conscious, he/she may not be responsive. The seizure can cause someone to slur his or her speech, make only noises, or lose the ability to vocalize completely.
In contrast to the typical perception of a seizure, many people in the ictal stage stop moving. Their muscles may lock up so their bodies tense and stiffen like a board. They may lose control of neck and head muscles, resulting in their heads slumping forward.
Other common physical signs of a seizure can include drooling, repeated eye movements, sweating, dilated pupils, increased heart rate, and loss of urinary or bowel control.
Stage 3: Postictal Stage
The postictal stage is the recovery phase, after the seizure occurs.
It is when the brain and body recover from the seizure. Recovery looks different for everyone: some people recover immediately and can continue to perform regular tasks, while others may take minutes or even hours to feel like their usual selves. The average postictal stage lasts for 5-30 minutes.
Many people with epilepsy report feeling disoriented during the period immediately after the seizure. People may remember nothing about the seizure or may have a distorted memory of the event, further contributing to this sense of disorientation.
Another common sensation is physical exhaustion. The post-seizure exhaustion may last for several days.
Types of Epileptic Seizures

One core element of this improved classification process is seizures are defined and categorized by where they start in the brain.33
Seizures that start in one area of the brain, are called focal seizures. Seizures that start in both sides of the brain, are called generalized seizures. Some seizures, begin as a focal seizure and then progress to generalized seizures.
A secondary component of the updated classification identifies whether a person’s awareness is affected during a focal seizure. This does not apply to generalized seizures, in which an individual’s awareness will be affected.
The third element of the updated classification structure is whether the person displays motor symptoms. Motor symptoms include what many commonly think of as a seizure: jerking, twitching, or stiffening movements of a body part. Non-motor symptoms include the less visible bodily changes such as changes in sensations, emotions, thoughts, and experiences.
Here’s what the new basic classification looks like:
Focal |
Generalized |
|---|---|
|
Aware or Impaired Awareness |
|
|
Motor and/or Non-Motor Symptoms |
Motor and/or Non-Motor Symptoms |
These distinctions are important because they enable medical professionals to better identify which medications should be used, whether surgery is a possible treatment, and assess possible causes of the seizure.
What is Temporal Lobe Epilepsy?
Approximately 60% of people with epilepsy can be classified as having temporal lobe epilepsy.
Temporal lobe epilepsy is characterized by a focal seizure which begins in the temporal lobe. Some of the temporal lobe’s primary functions include, comprehension, memory, and spatial navigation.
Patients experiencing a temporal lobe seizure report a wide range of experiences, from mild fascinations to mood swings. Like any focal seizure, seizures starting in the temporal lobe can expand their impact and affect the whole brain, becoming a generalized seizure.
Injury to the brain, either through head trauma or infection, are common causes of temporal lobe epilepsy.
Generalized Seizures
Generalized seizures involve both sides of the brain and muscle movements, usually not limited to one side of the body.
Generalized seizures nearly always result in impaired awareness and often in losing consciousness, either briefly or for a longer while.
Absence Seizures
Some generalized seizures are described as absence seizures. These are brief and non-convulsive. This type of seizure most often occurs in school-age children, and they can turn into a generalized tonic-clonic seizure. Absence seizures happen quickly and stop as fast. The seizures typically occur daily. People experiencing an absence seizure may appear to be unresponsive and their awareness may seem impaired. Symptoms frequently include:
- Blankly staring
- Eyelids fluttering
- Eyes rolling back in the head
- A fixed, blank stare
Generalized tonic-clonic seizures
Generalized tonic-clonic seizures are the seizures many people think of when they hear the word “epilepsy.” These seizures are marked by losing consciousness and stiffening or jerking of the muscles throughout the body. Any focal seizure can evolve into a generalized tonic-clonic seizure.
Status Epilepticus: The Most Serious Type of Seizure
Status Epilepticus is a prolonged generalized, or focal seizure, or a cluster of seizures that requires emergency treatment.34 Once the seizure or seizures are over, the victim is usually admitted to a hospital for recovery.
This form of seizure occurs in people with chronic epilepsy or may be a result of various medical conditions such as encephalitis, or meningitis.
Posttraumatic Epilepsy (PTE)
Head trauma causes 20% of all seizures. All forms of brain injury (mild, moderate, and severe) increase an individual’s risk of developing a seizure. Frequent causes include skull fractures and bleeding within the brain (brain hemorrhage). Even simple concussions or mild traumatic brain injury can cause a seizure to develop.35
Following head trauma, a seizure can develop within moments, but onset may be delayed for hours, days, or even weeks. Sometimes, however, a late onset seizure may not take place for months or even years.
The severity of the head trauma affects risk of future seizures.
These possible factors of a traumatic brain injury increase an individual’s risk of developing a seizure in their lifetime:
- Loss of consciousness or amnesia over 24 hours after trauma
- Experiencing an initial seizure during the first 24 hours after head trauma
- Experiencing a seizure during the first week after head trauma
- Age 65+ at time of trauma
- Children (particularly under 5)
- Subdural or intracerebral hematoma (bleeding within the brain)
- Depressed skull fracture (broken skull bone protruding into the brain)
- Difficulty following commands after a week
- Nonreactive pupil
- Damage to parietal lobe
- Metal or bone fragments in brain
Diagnosis
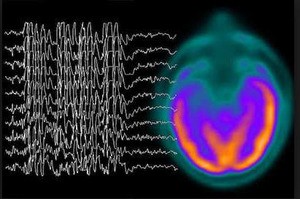
What is an EEG?36
The Electroencephalogram (EEG) is the test most frequently used by clinicians to diagnose a seizure. The test measures electrical impulses within the brain, but often the test results are normal because it is not being administered at the time an individual is experiencing a seizure.
When a seizure disorder is suspected, often, the patient will be hospitalized. Constant EEG monitoring of brain waves accompanied by video monitoring of the individual to capture and record a seizure taking place, can allow correlation of the video to and the EEG to determine the type and length of the seizure taking place.
Ambulatory EEG’s are also used to monitor patients suspected of having epilepsy. Patients can have recordings throughout the day while they are at home, work, or school.
Speaking with Your Doctor

Personal logs are often helpful to physicians in the diagnosis of post traumatic epilepsy.
It is recommended that individuals record any experiences (including duration and location of sensations).
When an individual’s symptoms correspond to a specific area of the brain, there is stronger evidence of epilepsy.
These symptoms can also occur in patients with epilepsy:
- Dream state (while awake)
- Dissociation (involuntary and disconnected memories, thoughts, or self-identity)
- Feelings of contact with higher being (religious experience)
- Slowed thinking
- Quickened thinking
- Altered experience of time
- Speech arrest (Inability to speak)
- Slurred, nonsensical, or repetitive speech
- Difficulty comprehending
- Dyslexia (difficulty reading or understanding symbols and words)
- Agraphia (inability to spell or write)
- Selective memory impairment
- Depression
- Random or over-the-top anger, pleasure, laughter, or crying
- Hypertension (elevated blood pressure)
- Peristalsis (involuntary intestinal contractions)
- Pallor (abnormally pale skin)
- Respiratory arrest
- Tachycardia (elevated heart rate)
- Sweating
- Urinary incontinence
- Mydriasis (dilated pupils)
- Unusual sleep movements (thrashing, screaming, thrusting, cursing, punching, and even bicycling)
- Intermittent or prolonged confusion or disorientation
Treatment
Antiepileptic Drugs (AEDs)
Once there is a diagnosis of epilepsy, the treatment goal is to control frequency and intensity of seizures while simultaneously decreasing other posttraumatic symptoms. Antiepileptic drugs (AEDs), are typically the first, and most effective choice. Because of the multitude of choices, side effects, and individual patient circumstances, the treatment options must be carefully analyzed.37
Doctors must first identify the area(s) of the brain in which seizures occur because different drugs target different areas. Then the individual symptoms must be identified for secondary treatment.
Doctors must balance an individual’s unique epileptic symptoms with a specific medication’s side effects, and symptoms from other health conditions (especially depression and anxiety) and their treatments’ side effects. Cognitive and behavioral evaluations are necessary to avoid compounding the epilepsy problems with adverse drug side effects.
Surgical Intervention
Is surgery an appropriate cure for epilepsy?
When prescription drugs are ineffective at controlling seizures, doctors may consider surgical intervention – usually combined with medication. Most epileptic surgical treatments target the damaged part of the brain that causes seizures, so patients whose seizures are focused in a certain region of the brain have a higher success rate than those who experience generalized seizures.
Resection (removal) surgery is historically the most successful because it removes the problem area.
Laser thermal ablation (LTA) recently emerged as an alternative to resection because it is less invasive. The technology uses a laser to melt or vaporize the problem area, rather than total removal. A probe can be inserted through a small hole in the cranium, which results in faster hospital discharge.
Vagus nerve stimulation (VNS) helps patients otherwise not able to benefit from surgery. This procedure is less invasive. The surgeon simply implants electrical stimulators directly on the problem area of the brain, allowing for continuous treatment. These stimulators help control seizures and can be adjusted in intensity to find the proper amount of electrical stimulation.
Responsive neurostimulation (RNS) is one of the most recently FDA approved methods providing hope to patients previously not considered for surgery. This method can stimulate neurons in the brain too deep for removal or disconnection and treat patients with multiple focal areas of the brain that cause seizures.
Marijuana Treatment for Epilepsy
Medical marijuana has been used to reduce the severity and frequency of seizures in limited human studies.38
Several states now approve medical marijuana to treat epilepsy. The marijuana used to treat epilepsy is different from that sold on the street. It is refined with only the therapeutic chemicals, CBD or THC remaining. THC is the psychoactive ingredient that causes the “high” recreational cannabis users seek. CBD is not psychoactive, so it induces no “high.” It does, however, have relaxation and anti-inflammatory effects, while possibly causing dry mouth, drowsiness, or lightheadedness.
On June 25, 2018, the U.S. Food and Drug Administration approved a new medication, Epidolex (cannabidol) for the treatment of patients with Dravet syndrome and Lennox-Gastaut syndrome. In multiple controlled studies the medication was shown to reduce the frequency of seizures.39
Dravet syndrome is a childhood genetic disorder. Fever related seizures appear in the first year of life followed by myoclonic seizures in later years.40
Lennox-Gastaut syndrome is also childhood seizure disorder characterized by frequent seizure activity that usually begins between ages 3 to 5.41
This is the first drug approved by the FDA for the treatment of seizure disorders.
Can Epilepsy be Cured?
While surgery that removes or vaporizes the affected area of the brain is the only procedure considered to “cure” epilepsy, it is not always an option – and not always curative. The good news is that other treatments can control most patients’ symptoms enough, so they may live normal lives. Patients and loved ones who familiarize themselves with the recognition of epileptic symptoms have a better chance of accurate diagnosis and successful treatment.
Having a precise idea of an individual’s epileptic symptoms help ensure that all needs are met. 70% of people with epilepsy achieve remission, and half of those with posttraumatic epilepsy (PTE) achieve remission within the first 15 years.42 Proper diagnosis and treatment is vital in improving management of the condition.
If you suffer or know someone who suffers from epilepsy, what can you do?

Keeping accurate notes of how a seizure develops and observations of the individual while they are having a seizure are important. There is never too much detail to record which may help your health care professional in diagnosing and treating the particular seizure. Additionally, the more you know about epilepsy and how it manifests itself, the better equipped you are to document symptoms to assist doctors’ understanding of your condition.
What is a Seizure Logbook?
Doctors may ask you to keep a log book of your symptoms to aid in diagnosis.43 Some important items to include in the log book include:
- What were you doing before signs or symptoms began?
- Were you fatigued, stressed, ill, or experiencing anything else unusual?
- How did the episode begin?
- How long does each involuntary feeling, movement, thought, or sensation last?
- How intense is the symptom relative to other experiences of this same symptom?
- In what ways did behavior change, or was there any unusual or involuntary behavior? (Behavioral status)
- In what ways did the ability to think, understand, or sense (touch, taste, smell, see, hear) information or stimuli change? (Cognitive status)
- Was the victim able to speak or respond to speech or touch?
- What sounds did the victim make?
- Where does each symptom physically occur on the body? (be specific)
- What other information do my doctors recommend that I observe and document?
- After the episode, what did the victim experience (fatigue, confusion, pain, etc.)?
Signs of Epilepsy in Children

Here are things to look for if you suspect a child may have epileptic symptoms:
- Abrupt stops in action
- Unresponsive for brief period, especially to touch or sound
- Abrupt return to action or responsiveness
- Staring
- Eye(s) rolling back
- Brief jerks, especially upon waking (can be single or multiple)
- Attempt to intentionally induce seizures (wave hand in front of face or move toward flashing lights)
- Repetitive motions (hand movements, bobbing head, blinking, licking, swallowing, sucking, chewing, bicycling or pedaling motion)
- Dilated pupils
- Flushed skin
- Elevated heart rate
- Salivation
- Unusually pale skin
- Rapid decrease in muscle tone
- Body goes limp
- Head nodding as eyes droop
- Loss of consciousness
- Sweating
- Tremors
- Losing urinary or bowel control
- Anxiety, depression, confusion, or drowsiness following any episode
- Stops breathing
- Muscles abruptly tighten or stiffen
- Spasms, especially prolonged over 5 seconds and in clusters
- Seeing, smelling, hearing, or feeling something that is not there (lights, numbness, enlarged vision)
- Goosebumps
- Sped or slowed breathing
- Memory loss
- Speech impairment
- Abrupt, random emotional outbursts
- Depersonalization (feeling outside one’s body)
- Déjà vu
- Feeling of knowing the future
- Fear
- Nausea
- Decrease in awareness
- Abrupt walking or running
- Repetitive speech
- Sudden screaming or thrashing, either while awake or asleep
- Daydreaming
- Behavioral changes or outbursts in specific situation(s)
If you suspect your child may have epilepsy, immediately call your doctor and communicate your specific concerns, so you can get an appointment as soon as possible and keep a log of all signs and symptoms you or your child observe.
Support for Sufferers of Epilepsy and Their Loved Ones

3 million people have epilepsy in this country, and millions more care for loved ones with epilepsy. Connect and participate in epileptic organizations and support groups for information and support.45
Legal Assistance following Post-Traumatic Epilepsy

Epilepsy victims frequently require expense specialized medications, emotional support, and other types of assistance. The time and financial resources to treat and manage epileptic seizures can be enormous and overwhelming.
Handling a case arising out of trauma, like an automobile accident, construction site accident, or a fall, resulting in posttraumatic epilepsy requires not only special knowledge about the injury, its causes, and applicable law, but caring and compassionate professionals who genuinely strive to allay your fears, answer your questions, and vigorously prosecute your claim.
How can you discover if an attorney possesses the knowledge and skills to represent victims of post traumatic epilepsy?
Ask them questions. Ask for more information and details about their background and experience in representing victims of head trauma. You are worthy of the best representation you can obtain for your case, so don’t be afraid to ask tough questions and look out for your interests.
Here are questions you should pose to an attorney before retaining him or her for your brain injury or epilepsy case:
- How many cases similar to mine have you been involved with as the principal attorney over the past three years?
- What percentage of your practice is devoted to representing persons with a traumatic brain injury?
- Have you ever represented someone with post-traumatic epilepsy or seizure disorder?
- Will you be handling my case personally or will you be referring it to another lawyer or law firm?
- What have been your results in representing persons with cases like mine?
- Have you written and published any articles on traumatic brain injury?
- Have you lectured to any bar associations, brain injury associations or other groups about the effective legal representation of persons with traumatic brain injury?
- Do you actively participate in your state’s brain injury association?
- Do you regularly attend conferences and read textbooks and articles about traumatic brain injury and post traumatic seizure disorder?
- Have you ever received any professional honors and awards about your representation of persons with a brain injury?
About De Caro & Kaplen, LLP
Shana De Caro and Michael V. Kaplen have devoted their professional practice to zealously advocating for victims of traumatic brain injury and post-traumatic epilepsy disorder. With knowledge, dedication, and compassion, Shana and Michael represent brain injury survivors throughout New York State and around the country.
At De Caro & Kaplen, LLP, we concentrate our practice on representing persons with brain injury. We frequently represent clients who have developed seizures and post-traumatic epilepsy because of their head injury. We are nationally recognized leaders in brain injury law. In over 40 years of practice, we have achieved verdicts and settlements in brain injury cases totaling over 100 million dollars.
Our attorneys have lectured to brain injury associations, lawyer’s groups, and medical associations on brain injury. They have authored articles published in legal publications, medical books, and journals on the legal aspects of traumatic brain injury and proper legal representation of brain injury victims. They have received many awards and honors for representation and advocacy on behalf of brain injury survivors.
We are honored that our senior partner, SHANA DE CARO serves as Chairwoman of the Brain Injury Association of America. Shana was also the first female chair of the Traumatic Brain Injury Litigation Group, which is devoted to representing victims of brain damage.
MICHAEL V. KAPLEN is a Professorial Lecturer in Law at the George Washington University Law School, teaching the only course devoted to traumatic brain injury law in the nation. He served three terms as president of the Brain Injury Association of New York State and chairs the prestigious New York State Traumatic Brain Injury Services Coordinating Council.
Our firm is the only firm in the United States whose two partners have both served as chairs of the American Association for Justice, Traumatic Brain Injury Litigation Group. Both of our attorneys have been selected as New York Super Lawyers. Shana De Caro and Michael Kaplen served as the attorneys for the Brain Injury Association of America in legal proceedings before the United States Third Circuit Court of Appeals and the United States Supreme Court objecting to and seeking to overturn the unjust settlement reached in the NFL class-action brain injury lawsuit.
About The Authors
This guide was co-authored by Shana De Caro & Michael V. Kaplen.
Shana De Caro is the Chairwoman of the Brain Injury Association of America. Michael V. Kaplen chairs the New York State Traumatic Brain Injury Services Coordinating Council and is past president of the Brain Injury Association of New York State. They have each chaired the Traumatic Brain Injury Litigation Group of the American Association for Justice and are co-authors of the “Current Issues in Neurolaw” Chapter in Traumatic Brain Injury: Defining Best Practice, Psychiatric Clinics of North America, members of the Advisory Board, Acquired Brain Injury Program, The George Washington University, Washington, D.C., Graduate School of Education and Human Development, and serve on the Board of Directors of the New York State Academy of Trial Lawyers.
- World Health Organization (WHO) “Epilepsy Fact Sheet” http://www.who.int/mediacentre/factsheets/fs999/en/
- Epilepsy Foundation: https://www.epilepsy.com/
- Silver, J., McAllister, T, Yudofsky, S. Textbook of Traumatic Brain Injury, 2nd Ed. American Psychiatric Publishing, Inc.,p. 266. https://psychiatryonline.org/doi/full/10.1176/appi.books.9781585624201.js16
- Silver, J., McAllister, T, Yudofsky, S. Textbook of Traumatic Brain Injury, 2nd Ed. American Psychiatric Publishing, Inc., p. 266. https://psychiatryonline.org/doi/full/10.1176/appi.books.9781585624201.js16
- Silver, J., McAllister, T, Yudofsky, S. Textbook of Traumatic Brain Injury, 2nd Ed. American Psychiatric Publishing, Inc., p. 266. https://psychiatryonline.org/doi/full/10.1176/appi.books.9781585624201.js16
- American Brain Tumor Association https://www.abta.org/about-brain-tumors/brain-tumor-signs-symptoms/
- American Stroke Association. Seizures and Strokes http://www.stroke.org/we-can-help/survivors/stroke-recovery/post-stroke-conditions/physical/seizures-and-epilepsy
- World Health Organization (WHO) “Epilepsy Fact Sheet” http://www.who.int/mediacentre/factsheets/fs999/en/
- https://www.brainline.org/article/seizures-and-traumatic-brain-injury
- Frey LC (2003). “Epidemiology of posttraumatic epilepsy: A critical review”. Epilepsia 44 (Supplement 10): 11–17. https://www.ncbi.nlm.nih.gov/pubmed/14511389
- World Health Organization (WHO) “Epilepsy Fact Sheet” http://www.who.int/mediacentre/factsheets/fs999/en/
- NYU Langone Health. Types of Epilepsy & Seizure Disorders in Adults. https://nyulangone.org/conditions/epilepsy-seizure-disorders-in-adults/types
- Mayo Clinic. Seizure Symptoms https://www.mayoclinic.org/diseases-conditions/seizure/symptoms-causes/syc-20365711
- Centers for Disease Control and Prevention (CDC). Epilepsy. Data and Statistics: https://www.cdc.gov/epilepsy/data/index.html
- Epilepsy Foundation. Who Gets Epilepsy? https://www.epilepsy.com/learn/about-epilepsy-basics/who-gets-epilepsy
- Meacham, J. Newsweek. Epilepsy: Overlooked and Underfunded http://www.newsweek.com/epilepsy-overlooked-and-underfunded-77467
- Centers for Disease Control and Prevention (CDC) More Persons Have Epilepsy Than Ever Before. https://www.cdc.gov/media/releases/2017/p0810-epilepsy-prevalence.html
- http://keranews.org/post/what-you-should-know-about-epilepsy
- Centers for Disease Control and Prevention. Sudden Unexpected Death in Epilepsy (SUDEP) https://www.cdc.gov/epilepsy/about/sudep/index.htm
- Centers for Disease and Prevention (CDC). Epilepsy: Fast Facts https://www.cdc.gov/epilepsy/about/fast-facts.htm
- Epilepsy Foundation. What Causes Epilepsy https://www.epilepsy.com/learn/about-epilepsy-basics/what-causes-epilepsy-and-seizures
- Silver, J., McAllister, T, Yudofsky, S. Textbook of Traumatic Brain Injury, 2nd Ed. American Psychiatric Publishing, Inc., p. 266. https://psychiatryonline.org/doi/full/10.1176/appi.books.9781585624201.js16
- Silver, J., McAllister, T, Yudofsky, S. Textbook of Traumatic Brain Injury, 2nd Ed. American Psychiatric Publishing, Inc., p. 266. https://psychiatryonline.org/doi/full/10.1176/appi.books.9781585624201.js16
- World Health Organization (WHO) “Epilepsy Fact Sheet” http://www.who.int/mediacentre/factsheets/fs999/en/
- World Health Organization (WHO) “Epilepsy Fact Sheet” http://www.who.int/mediacentre/factsheets/fs999/en/
- World Health Organization (WHO) “Epilepsy Fact Sheet” http://www.who.int/mediacentre/factsheets/fs999/en/
- Epilepsy Foundation Triggers of Seizures https://www.epilepsy.com/learn/triggers-seizures
- Epilepsy Foundation Photosensitivity and Seizures. https://www.epilepsy.com/learn/triggers-seizures/photosensitivity-and-seizures
- Epilepsy Foundation What Happens During A Seizure? https://www.epilepsy.com/learn/about-epilepsy-basics/what-happens-during-seizure
- University of Chicago Medical Center. Stages of a seizure http://www.uchospitals.edu/specialties/neurosciences/epilepsy/seizure/stages.html; Epilepsy Foundation What Happens During A Seizure? https://www.epilepsy.com/learn/about-epilepsy-basics/what-happens-during-seizure
- Centers for Disease Control and Prevention. Types of Seizures https://www.cdc.gov/epilepsy/about/types-of-seizures.htm
- International League Against Epilepsy (ILAE) Operational classification of seizure types by the International League Against Epilepsy: Position Paper of the ILAE Commission for Classification and Terminology https://onlinelibrary.wiley.com/doi/full/10.1111/epi.13670; Epilepsy Foundation New Terms for Seizure Classification https://www.epilepsy.com/learn/types-seizures/new-terms-seizure-classification
- NYU Langone Health. Types of Epilepsy & Seizure Disorders in Adults https://nyulangone.org/conditions/epilepsy-seizure-disorders-in-adults/types
- Johns Hopkins School of Medicine Status Epilepticus https://www.hopkinsmedicine.org/healthlibrary/conditions/nervous_system_disorders/status_epilepticus_134,42
- Silver, J., McAllister, T, Yudofsky, S. Textbook of Traumatic Brain Injury, 2nd Ed. American Psychiatric Publishing, Inc. https://psychiatryonline.org/doi/full/10.1176/appi.books.9781585624201.js16; Zasler, ND, Katz, DI. Zafonte, RD. Brain Injury Medicine Principles and Practices, 2nd Ed. Demos Medical https://web.archive.org/web/20180927224110/http://www.springerpub.com/brain-injury-medicine-2nd-edition-9781936287277.html
- U.S. Dept. of Veterans Affairs. Epilepsy Centers of Excellence. What is an electroencephalography (EEG)? https://www.epilepsy.va.gov/Information/about.asp#diagnose
- National Institutes of Neurological Disorders and Stroke. The Epilepsies and Seizures: Hope Through Research https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Hope-Through-Research/Epilepsies-and-Seizures-Hope-Through#3109_32
- Epilepsy Foundation Medical Marijuana and Epilepsy https://www.epilepsy.com/learn/treating-seizures-and-epilepsy/other-treatment-approaches/medical-marijuana-and-epilepsy
- FDA approves first drug comprised of an active ingredient derived from marijuana to treat rare, severe forms of epilepsyhttps://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm611046.htm
- What is Dravet Syndrome? https://www.dravetfoundation.org/what-is-dravet-syndrome/
- Lennox-Gastaut Syndrome https://www.epilepsy.com/learn/types-epilepsy-syndromes/lennox-gastaut-syndrome-lgs
- Epilepsy Society The Prognosis for Epilepsy https://www.epilepsysociety.org.uk/sites/default/files/attachments/Chapter36Neligan2015.pdf; Ventola CL. Epilepsy Management: Newer Agents, Unmet Needs, and Future Treatment Strategies. Pharmacy and Therapeutics. 2014;39(11):776-792. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4218673/
- Epilepsy Foundation Seizure Information Forms. https://www.epilepsy.com/living-epilepsy/toolbox/seizure-information-forms
- The Hospital for Sick Children Signs and Symptoms of Seizures http://www.aboutkidshealth.ca/En/ResourceCentres/Epilepsy/AboutEpilepsy/Pages/Signs-and-Symptoms-of-Seizures.aspx
- Epilepsy Foundation: https://www.epilepsy.com/; Finding a Cure for Epilepsy and Seizures (FACES): http://faces.med.nyu.edu/; Brain Injury Association of America: https://www.biausa.org