In a presentation to the North American Brain Injury Association Medical/Legal Seminar, Michael V. Kaplen discusses the future of TBI litigation.

In 1981 when the Head Injury Association was formed, a head injury or a brain injury was not on anyone’s radar screen, unless you were the parent or the spouse of an individual whose was spared by advances in medical technology and surgical care.
Concussions were viewed as a bump on the dead and most failed to recognize a concussion as a brain injury.
So now 40 years later, the question is, where are we and what does the future hold for much brain injury, both acquired and traumatic?
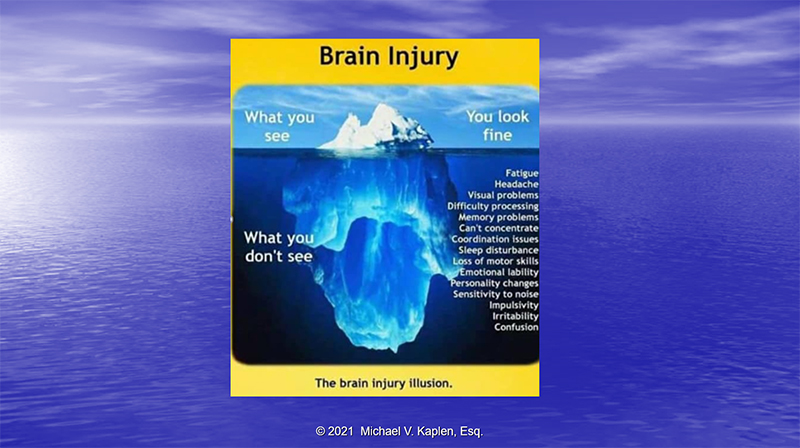
The illusion of brain injury remains the same across all spectrums of brain damage.
You Look fine.
You Sound fine.
So, you must be fine.
But what you do not see continues to be the dilemma and the frustration of brain injury survivors.
The frustration faced by brain injury survivors, the questioning by family members and friends and by insurance carriers, defense doctors, and the judicial system compounds the difficulty that persons with a brain injury have in trying to pick up the pieces and resume their lives.
From the outside looking in, you can never understand.
From the inside looking out, you can never explain it.
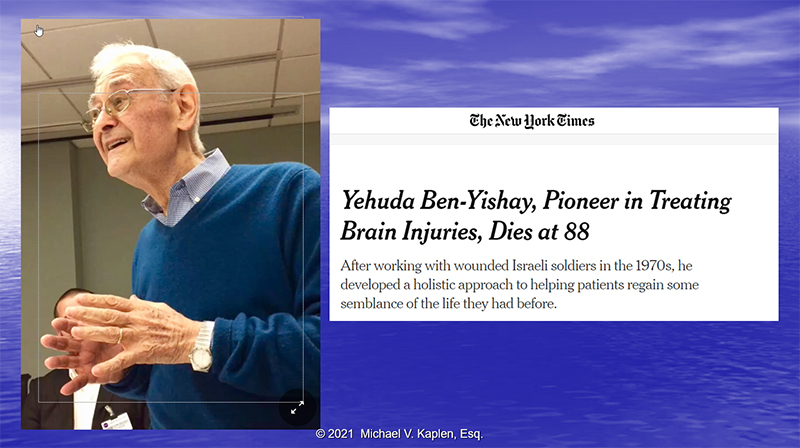
I want to pay tribute to a dear friend, Dr. Yehuda Ben Yishay, someone who understood this dilemma and asked the still most important question:
Can you reconstruct Humpty Dumpty after he or she has been shattered to pieces?
Yehuda understood that to heal a brain injury required more that physical healing to brain. Healing and rehabilitation must consider the emotional well-being of the individual to be effective.
“Once brain injured, you are always injured for the rest of your life,” Yehuda told the New York Times in a 2006 interview, But, persistence courage, acceptance and finding was to compensate are the path to recovery. Something that we cannot afford to lose sight of as we look to what is ahead.

In 1986, 5 years after the Head Injury Association and its affiliate, the Head Injury Association of New York State were formed by parents attempting to figure out how to obtain services, how to access in state services, how to bring their children home from institutions, and how to pay for services, the State of New York issued a damning a report on the quality and availability of services to brain injury survivors and their families in New York.
The conclusion was a clarion call to all:
There was:
- No coordination of services
- No defined state policies
- No comprehensive network of support or assistance.
As Dr. Greg O’Shanick, medical director of the Brain Injury Association of America had said, “As awareness of TBI has grown, more people are seeking treatment, but patient’s may receive incomplete information and follow up treatment can be spotty”.
Unfortunately, the same issues identified in the 1986 report to the Governor still remain unresolved and until we address these issues of services, coordination, and support, nothing will change.

Brain Injury is a public health crisis. It is a national emergency.
Just look at these statistics.
We used to say a brain injury every 30 seconds, then we updated to say every 15 seconds.
The latest epidemiological studies find a brain injury occurs to someone every 9 seconds.
Brain injury has reached pandemic proportions.
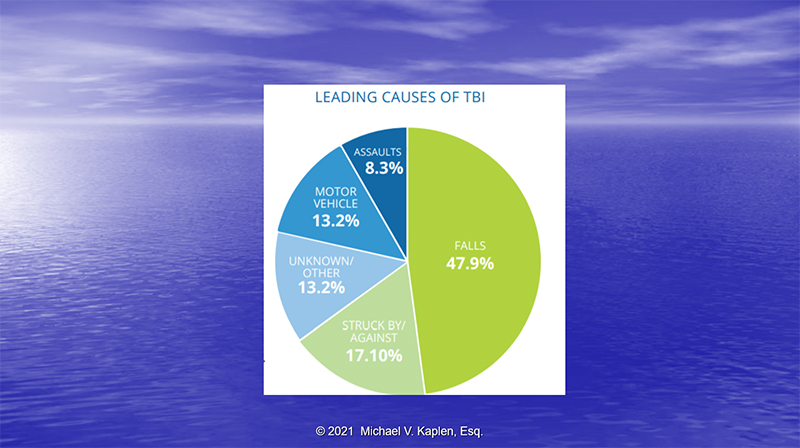
Current epidemiological research finds that Falls are the lead cause of brain injury in the United States today and there has been a clear shift to older individuals who are more prone to calls. The severity in these individuals is greater and more deaths are seen. More attention must be devoted to preventing these falls from occurring both in and out of the home; in nursing homes and hospitals were falls are described as never events, greater care must be taken to prevent patient’s from falling. Sidewalks and walkways must be properly maintained. Proper building maintenance is essential.
Air bags, seat belts, car seats, collision avoidance technology in vehicles has caused a decline in brain injury caused by vehicular crashes, but that does not mean that brain injury is on the decline.
But the rate of intimate partner violence is on the rise and the CDC reports that 90 percent of all victims of intimate partner violence have sustained a brain injury! But sadly many cases go unrecognized and untreated. This must stop. Hospital emergency departments and police agencies must be made aware of brain injury in this group and they must properly identify these individuals so proper treatment can be provided.
Today and tomorrow, the Best cure for a brain injury continues to be prevention.

Covid 19 has produced a new class of brain injury survivors.
It is called Neuro-Covid or Covid Brain Fog.
The neuropsychological impact of Covid-10 includes sleep impairment, anxiety, memory impairment, anxiety, depression, headaches, cognitive fatigue.
Covid 19 has been associated with an increased risk of intracranial hemorrhage, and dementia.
It is too early to describe the full clinical picture of post Covid neurological symptoms, but without a doubt, Covid 19 will increase the burden of caring for brain injury survivors.
And yet, with a brain injury occurring to someone in the US every 9 seconds, there are still some who are living in an alternative universe. This attitude toward brain injury survivors is not only disrespectful, it is disgraceful.
Looking into the future, Bio-chemical markers in the blood hold great promise for rapid diagnosis and rapid treatment of a concussion.
It is the future of sports concussion management and return to play decision making. The technology also holds promise for predictions about brain injury recovery and assessment of our military personnel who frequently go undiagnosed and untreated following a concussion.
An objective marker of brain injury is an important and exciting development with traumatic brain injury identification, diagnosis, and treatment.
TBI diagnosis today is still very much a clinical diagnosis. Objective proof of brain injury is much needed to protect the rights of brain injury survivors both in and out of the judicial system. We can no longer afford to rely on the Glasgow coma scale and its classification of brain injury.
Diffusion Tensor Imaging (DTI); Positive Emission Tomography (DTI) and promising new technology known as Magnetoencephalography (MEG) are leading the way to provide this objective documentation of the injured brain.
As sensitivity and specificity improve, more reliance will be placed upon these tools in the clinical setting to assist in diagnosis and treatment.
But we cannot forget that the best test for brain injury and brain damage is life itself.
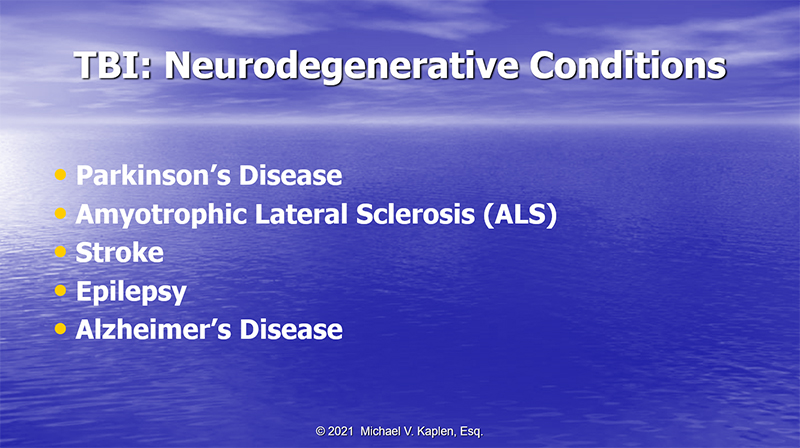
There continues to be increasing evidence that head trauma is a cause of these neurodegenerative conditions.
No discussion of traumatic brain injury can take place in the year 2021 without reference to Chronic Traumatic Encephalopathy (CTE). CTE is the leading issue in sports medicine today and will continue to be.
CTE has fueled debate about the need to curtail tackle football in our children and how to compensate athletes but professional and amateur who have contracted this condition.
Brain injury is a complex medical issue and a chronic medical condition.
Evidence continues to mount about the effect of brain injury on the entire body and conditions such as:
- Hypertension
- Obesity
- Endocrine Disorders
- Sleep Disorders
- Alcoholism
- Substance Abuse
- Depression
Evidence continues to mount that the effects of a traumatic brain injury can and will last a lifetime and affect both work life expectancy and life expectancy.
In professional and amateur sports, sports concussion management issues continue to predominate including questions about the very definition of what is a concussion; how is it diagnosed; when can a player safely be allowed to return to play following a concussion; return to learn and the class room including accommodations and the effect of repetitive head trauma.
There continues to be updated sports concussion management legislation and court decisions on this legislation to define both duty and liability for failing to comply with legislative mandates.

No discussion on TBI Litigation and the future would be complete without reference and an update on the NFL Class Action Lawsuit and its settlement.
The latest twist on the settlement and further proof this settlement was not entered into with the best interest of all the players, is the revelation that the settlement administrator is using something known as Race-Norming to adjust the scoring of player’s neuropsychological assessments for dementia to determine if they are eligible for compensation under the settlement.
Both sides, the NFL and the attorneys supposedly representing all players, originally agreed to use race norming which inherently presumes a lower cognitive baseline for Black individuals in general and black players. This translates into the racially discriminatory assumption that Black players have lower cognitive abilities then their white counterparts making it more difficult to obtain benefits when comparing a players current condition to the presumed norm.
Why the attorneys for the players ever agreed to this racist grading scale is beyond me. But they now have had a change in heart after this scoring was revealed by independent attorneys for some players who were denied compensation based on these norms. All sides, the NFL and the attorneys for the class action players have been ordered to mediation to deal with the issues. Both sides have agreed not to use this racist criterion in future assessments, but the issue remains unresolved regarding what to do with players denied compensation using this standard.
Why there has been no agreement on re-evaluating these players based on the same criteria used by the administrator in looking at white players is the question that still needs to be answered.
In the most recent development this week, the District Court has imposed a gag order on all sides participating in the mediation to resolve race norming.
Covid 19 has opened the door to new ways and methods of evaluating individuals with brain injury and new treatment possibilities.
One difficulty faced by many brain injury survivors is access to care. Whether because individuals live in rural areas where care is not accessible and simply not existent or because of lack of transportation for others, telemedicine has now become the new normal for many in the evaluation and treatment of brain injury survivors.
Translated into litigation, issues such as video taping defense neuro psychological examinations and the position of defense forensic examiners and their associations will need to be reassessed by the Courts. After all if you can perform these evaluations remotely for treatment, why are they taboo for litigation?
At the conclusion of the case, subrogation issues still haunt the ability to compensate our clients.
Unfortunately, US Airways v. McCutchen is still the law and ERISA plans have been afforded the right to be first in line following a settlement before case disbursements, before attorney fees and without regard to the equitable made whole principle.
Michael V. Kaplen, is a partner in the New York brain injury law firm De Caro & Kaplen, LLP, and chairs the New York State Traumatic Brain Injury Services Coordinating Council.
